Hematologic Diseases
Cleveland Clinic Laboratories offers a full range of expert consultative services to provide clients with expert diagnosis and treatment of hematologic diseases.
Diseases include acute lymphoblastic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, myeloproliferative neoplasms, myelodysplastic syndromes, Non-Hodgkin lymphomas, and plasma cell myeloma.
Interested in requesting a pathology consult? Our expert Hematopathology staff is available to answer clients’ questions throughout the entire consultation process.
Laboratory Medicine
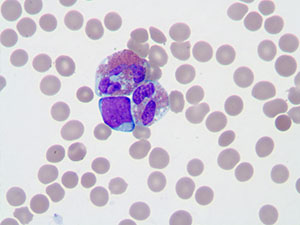
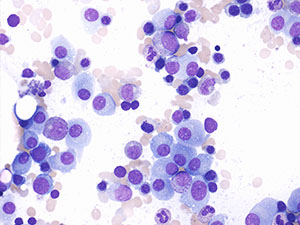
Acute Lymphoblastic Leukemia
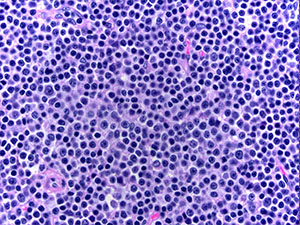
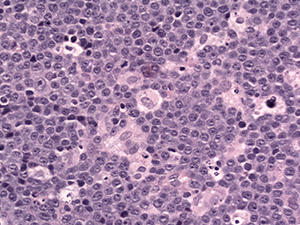
Acute lymphoblastic leukemia (ALL) is primarily a disease of childhood, with the majority of cases occurring before age six.
Acute lymphoblastic leukemia can be further subclassified based on the phenotypic profile and the presence of specific recurrent cytogenetic abnormalities. Approximately 80% of acute lymphoblastic leukemia exhibit a precursor B cell phenotype, with the remaining cases displaying a T lymphoblast phenotype.
Interphase fluorescence in situ hybridization (FISH) studies offer the ability to rapidly detect cytogenetic abnormalities in nondividing cells and are an important adjunct to traditional banded karyotyping. FISH analysis can clarify suspected abnormalities identified in banded karyotypes, identify the presence of complex or cryptic cytogenetic abnormalities, or provide cytogenetic information even when banded karyotype data is not available. FISH studies for recurrent cytogenetic abnormalities associated with B lymphoblastic leukemia are available through Cleveland Clinic Laboratories.
Single nucleotide polymorphism (SNP) arrays offer the potential to identify chromosomal abnormalities, including copy neutral loss of heterozygosity (cnLOH), which are not detected by metaphase cytogenetics and may also impact the classification and prognosis of acute lymphoblastic leukemia.
Real-time PCR testing offers the ability to detect oncogenic fusion transcripts with a sensitivity much greater than that obtained with other techniques, such as metaphase cytogenetics or FISH. In Philadelphia chromosome-positive acute lymphoblastic leukemia, RT-PCR analysis for p190 BCR / ABL transcripts is utilized to monitor minimal residual disease status.
Testing Recommendations for Acute Lymphoblastic Leukemia (ALL):
BCR / ABL Qualitative Multiplex RT-PCR
BCR / ABL p190 RT-PCR, Quantitative
Bone Marrow Cancer Microarray & SNP
CC-SIGN™ Hematologic Neoplasm NGS Panel
• Subpanel: CC-SIGN™ Acute Lymphoblastic Leukemia (ALL) Panel
Chromosome Analysis: Bone Marrow or Leukemic Blood
DNA Extraction
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
Fluorescence in situ hybridization (FISH) for:
• MLL (11q23) Translocation
• t(12;21) ETV6 / RUNX1 (TEL / AML1)
• t(9;22) BCR / ABL1
• Trisomy 4 & 10
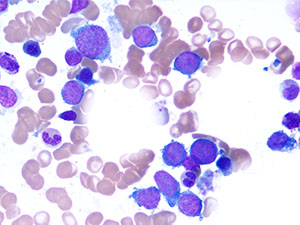
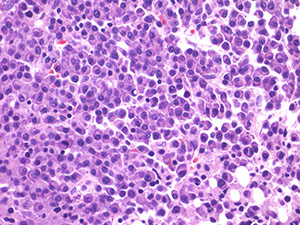
Acute Myeloid Leukemia
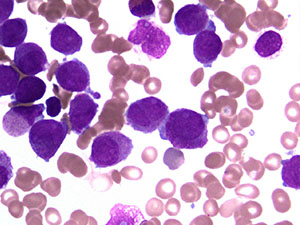
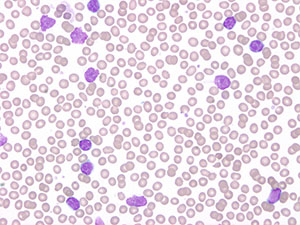
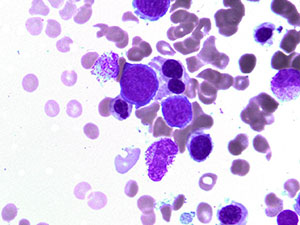
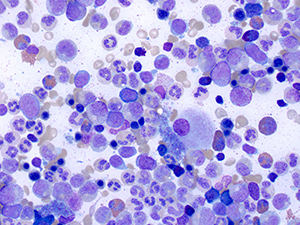
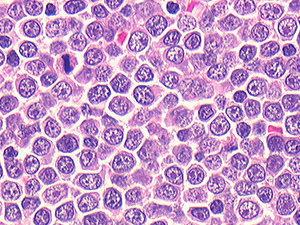
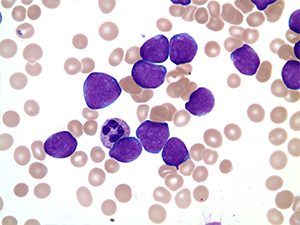
Acute myeloid leukemia (AML) is a malignant neoplasm characterized by the clonal proliferation of myeloid blasts in the peripheral blood and bone marrow.
Acute myeloid leukemia is clinically-heterogeneous and can be further subclassified through the correlation of clinical data, morphology, phenotype, and molecular cytogenetic abnormalities.
Metaphase cytogenetic analysis has long been recognized as a crucial component of the diagnosis and classification of acute myeloid leukemia; however, in recent years, other molecular methods have also assumed an increasingly important role in the workup, classification, prognostic assessment, and monitoring of acute myeloid leukemia.
Interphase fluorescence in situ hybridization (FISH) studies offer the ability to rapidly detect cytogenetic abnormalities in nondividing cells and are an important adjunct to traditional banded karyotyping. FISH analysis can clarify suspected abnormalities identified in banded karyotypes, identify the presence of complex or cryptic cytogenetic abnormalities, or provide cytogenetic information even when banded karyotype data is not available. FISH studies for many recurrent cytogenetic abnormalities associated with acute myeloid leukemia are available through Cleveland Clinic Laboratories.
Molecular testing for specific recurrent mutations is also an important part of the workup of acute myeloid leukemia. A next-generation sequencing panel identifies mutations that are of diagnostic or prognostic significance in acute myeloid leukemia. Single nucleotide polymorphism (SNP) arrays offer the potential to identify chromosomal abnormalities, including copy neutral loss of heterozygosity (cnLOH), which are not detected by metaphase cytogenetics and may also impact the classification and prognosis of acute myeloid leukemia.
RT-PCR testing offers the ability to detect oncogenic fusion transcripts with a sensitivity much greater than that obtained with other techniques, such as metaphase cytogenetics or FISH. In acute promyelocytic leukemia, RT-PCR analysis for PML / RARA transcripts is utilized to monitor minimal residual disease status.
Testing Recommendations for Acute Myeloid Leukemia (AML):
Bone Marrow Cancer Microarray & SNP
CEBPA Mutation Analysis
CC-SIGN™ Hematologic Neoplasm NGS Panel
Chromosome Analysis: Bone Marrow or Leukemic Blood
DNA Extraction
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
FLT3 ITD / D835 PCR
KIT Gene Mutation
NMP1 Mutation Analysis
PML / RARA RT-PCR, Qualitative
Fluoresence in situ hybridization (FISH) for:
• Acute Myeloid Leukemia Panel (t(8;21), inv(16), t(15;17), MLL)
• inv(16) CBFB / MYH11
• MLL (11q23) Translocation
• RARA (17q21) Translocation
• t(15;17) PML / RARA
• t(8;21) RUNX1 / RUNX1T1 (AML1 / ETO)
• t(9;22) BCR / ABL1
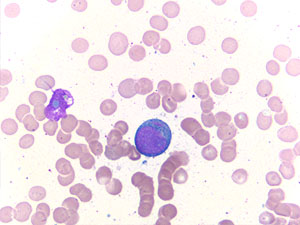
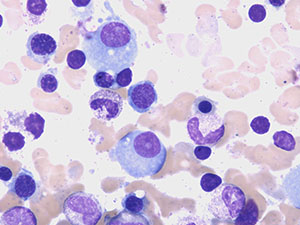
Chronic Lymphocytic Leukemia
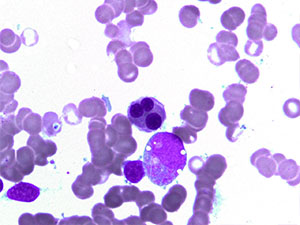
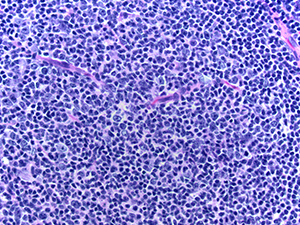
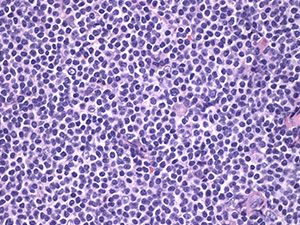
Chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL) is a neoplasm of small B lymphocytes that involves the peripheral blood, bone marrow, and, in some cases, the lymph nodes.
Most patients with chronic lymphocytic leukemia are older than 50 years of age, and most cases will follow an indolent clinical course.
FISH testing for recurrent cytogenetic abnormalities (13q-, +12, 11q-, and 17p-) provides important prognostic information in chronic lymphocytic leukemia.
The Oncologic CytoScan™ HD SNP Array assay assesses for chromosomal copy number abnormalities and loss of heterozygosity across the genome, including loci not covered by FISH panels.
PCR and sequencing analysis of the immunoglobulin heavy chain variable region (IGVH) can also provide further prognostic information.
Testing Recommendations for Chronic Lymphocytic Leukemia (CLL):
CC-SIGN™ Hematologic Neoplasm NGS Panel
Chromosome Analysis: Bone Marrow or Leukemic Blood
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
IGVH Sequencing
Oncologic CytoScan™ HD SNP Array
Fluorescence in situ hybridization (FISH) for:
• CLL (13q, +12, 11q, 17p)
Myeloproliferative Neoplasms
Myeloproliferative neoplasms are clonal hematological disorders characterized by an abnormal proliferation of one or more myeloid lineages in the peripheral blood.
Traditionally, four subtypes of myeloproliferative neoplasms have been recognized: chronic myeloid leukemia (CML), polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
More recently, three additional disorders have been identified that are identified by chromosomal rearrangements involving the PDGFRA, PDGFRB, or FGFR1 genes.
In chronic myeloid leukemia, molecular testing is utilized in several ways:
- First, chronic myeloid leukemia carries a BCR / ABL translocation, which can be identified through metaphase cytogenetics, FISH, or RT-PCR analysis.
- Secondly, following the initiation of therapy for chronic myeloid leukemia, minimal residual disease status is monitored utilizing qualitative multiplex RT-PCR analysis for the p210 BCR / ABL fusion transcript.
- Finally, sequencing of the BCR / ABL kinase domain can identify mutations associated with resistance to one or more tyrosine kinase inhibitors, thereby assisting in the selection of the most appropriate therapeutic option for the patient.
Molecular testing also plays an important role in non-chronic myeloid leukemia myeloproliferative neoplasms:
- JAK2 V617F mutations are found in >95% of polycythemia vera and in approximately 50% of essential thrombocythemia and primary myelofibrosis.
- In the rare cases of polycythemia vera lacking the V617F mutation, other mutations in exons 12–15 of JAK2 may be identified by sequencing studies.
- Mutations involving the CALR or MPL genes are identified in most cases of primary myelofibrosis or essential thrombocythemia lacking the JAK2 V617F mutation.
- A myeloid mutation panel by Next-Generation Sequencing (NGS) also detects numerous other mutations that may be of diagnostic or prognostic significance in myeloproliferative neoplasms.
- FISH testing can be utilized to detect chromosomal rearrangements in PDGFRA, PDGFRB, or FGFR1 that define distinct myeloproliferative neoplasms.
Testing Recommendations for Myeloproliferative Neoplasms (MPN):
BCR / ABL Kinase Domain Sequencing RT-PCR
BCR / ABL Qualitative Multiplex RT-PCR
BCR / ABL p190 RT-PCR, Quantitative
CALR Mutation Analysis
CC-SIGN™ Hematologic Neoplasm NGS Panel
Chromosome Analysis: Bone Marrow or Leukemic Blood
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
JAK2 Exon 12-15 Sequencing
JAK2 V617F PCR
KIT (D816V) Mutation by PCR
MPL Mutation Sequencing
Oncologic CytoScan™ HD SNP Array
Fluorescence in situ hybridization (FISH) for:
• FGFR1 (8p12) Translocation
• Myeloproliferative Neoplasms Panel (BCR / ABL1, PDGFRA, PDGFRB, FGFR1)
• PDGFRA (4q12) Translocation
• PDGFRB (5q32) Translocation
• t(9;22) BCR / ABL
Myelodysplastic Syndromes
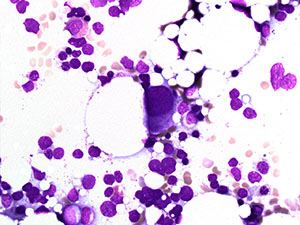
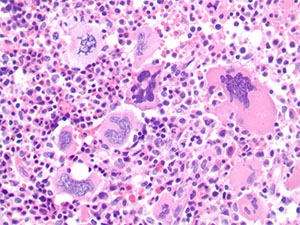
Myelodysplastic syndromes (MDS) are clonal hematologic malignancies characterized by ineffective hematopoiesis and peripheral blood cytopenias.
Myelodysplastic syndromes typically present in the middle age to elderly age groups. The diagnosis and subclassification of myelodysplastic syndromes is facilitated by detection of cytogenetic abnormalities, with the most common abnormalities being 5q-, 7q-, +8, and 20q-.
Interphase fluorescence in situ hybridization (FISH) studies offer the ability to rapidly detect cytogenetic abnormalities in nondividing cells and are an important adjunct to traditional banded karyotyping. FISH analysis can clarify suspected abnormalities identified in banded karyotypes, identify the presence of complex or cryptic cytogenetic abnormalities, or provide cytogenetic information even when banded karyotype data is not available.
FISH studies for many recurrent cytogenetic abnormalities associated with myelodysplastic syndromes are available through Cleveland Clinic Laboratories. SNP array karyotyping is also useful to identify clinically-significant chromosomal abnormalities which may be missed by metaphase cytogenetics and/or FISH studies alone.
Testing Recommendations for Myelodysplastic Syndromes (MDS):
Bone Marrow Cancer Microarray & SNP
CC-SIGN™ Hematologic Neoplasm NGS Panel
Chromosome Analysis: Bone Marrow or Leukemic Blood
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
Fluorescence in situ hybridization (FISH) for:
• Del(5q) Abnormalities
• Myelodysplasia (MDS) (5q,7q,+8,20q)
Non-Hodgkin Lymphoma
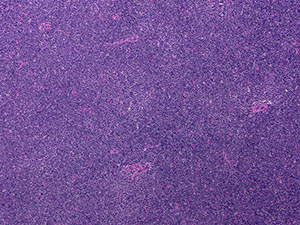
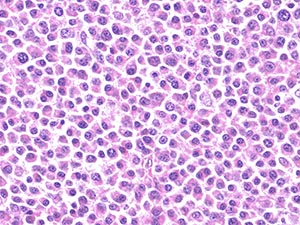
Non-Hodgkin lymphomas (NHL) are a heterogeneous group of malignancies of mature B-cells or T-cells.
Non-Hodgkin lymphomas are subclassified into distinct clinicopathologic entities on the basis of clinical features, morphology, phenotype, and molecular cytogenetic findings.
Approximately 90% of Non-Hodgkin lymphomas are derived from B-cells, with the remaining 10% being of T-cell origin. On average, Non-Hodgkin lymphoma typically presents in adults in their sixth or seventh decade, although some specific subtypes of Non-Hodgkin lymphomas occur more commonly in children or young adults.
Molecular testing is useful to document the presence of a clonal B-cell or T-cell population in the workup of a suspected Non-Hodgkin lymphoma. Historically, Southern blot studies have been considered to be the gold standard for documentation of clonal lymphoid populations; however, Southern blot studies require fresh or frozen tissue, and cannot be performed on formalin-fixed, paraffin embedded (FFPE) tissues. PCR studies utilizing primer sets designed by the EuroClonality (BIOMED-2) consortium offer the ability to detect clonal populations with a sensitivity approximately equal to that of Southern blot techniques, even from FFPE tissues.
Several subtypes of Non-Hodgkin lymphoma are characterized by specific recurring balanced translocations. These abnormalities may be detected by fluorescence in situ hybridization or by RT-PCR.
In general, FISH testing is considered the gold standard for detection of these abnormalities at initial diagnosis. FISH testing for Non-Hodgkin lymphoma-associated abnormalities can be performed on peripheral blood, bone marrow, or FFPE tissues.
Testing Recommendations for Non-Hodgkin Lymphomas (NHL):
B-cell Clonality Using BIOMED-2 PCR Primers (IGH + IGK)
B-cell Clonality, Tier 2 (BIOMED IGH DJ + IGL)
Chromosome Analysis, Solid Tumor
Flow Cytometric Immunophenotyping for Lymphoma, Tissue
Immunoglobulin Heavy Chain Using BIOMED-2 PCR Primers
IGH / BCL2 PCR, Qualitative
Immunoglobulin Kappa Chain Using BIOMED-2 PCR Primers
MYD88 L265P Mutation Analysis
Oncologic CytoScan™ HD SNP Array
T-Cell & B-Cell Clonality Using BIOMED-2 Primers (TCRB + TGRG)
T-Cell Receptor Beta Using BIOMED-2 Primers
T-Cell Receptor Delta Using BIOMED-2 Primers
T-Cell Receptor Gamma (TCRG) Using BIOMED-2 Primers
Fluorescence in situ hybridization (FISH) for:
• ALK (2p23) Translocations
• BCL2 (18q21.3) Translocations
• BCL6 (3q27) Translocations
• CCND1 (11q13) Translocation
• IGH/MALT1 (18q21) Translocation
• MYC (8q24) Translocation
• t(8;14) IGH / MYC
• t(11;14) IGH / CCND1
• t(11;18) BIRC3/ MALT1
• t(14;18) IGH / BCL2
• t(14;18) IGH / MALT1
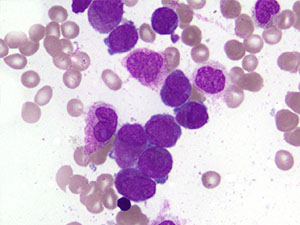
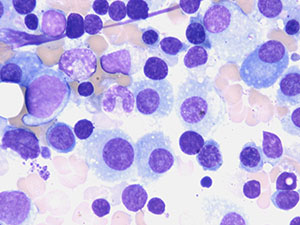
Plasma Cell Myloma
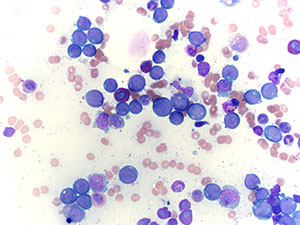
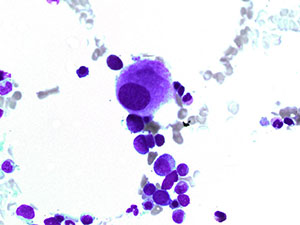
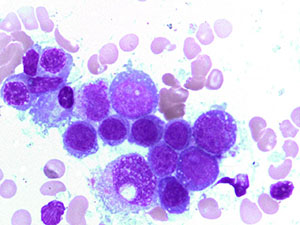
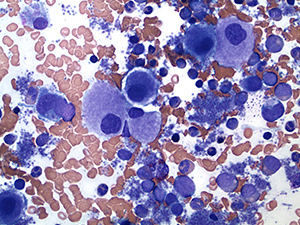
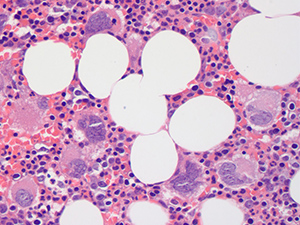
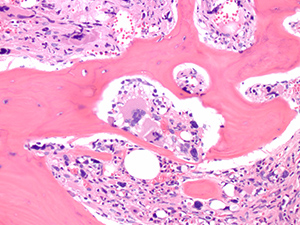
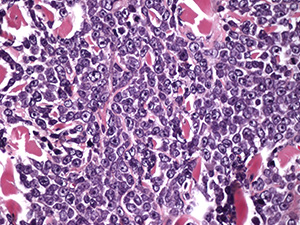
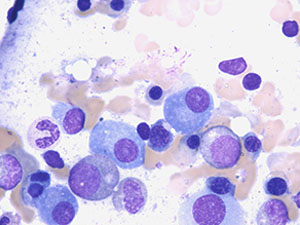
Plasma cell myeloma (PCM) is a malignant neoplasm of plasma cells characterized by increased plasma cells in the bone marrow and production of a monoclonal protein in the serum and/or urine.
The diagnosis of plasma cell myeloma is based on a combination of clinical findings, bone marrow aspirate and biopsy, and radiographic studies.
The clinical course of plasma cell myeloma is highly variable. FISH studies for recurrent cytogenetic abnormalities, including 13q, 17p-, IGH / CCND1, IGH / MMSET, and IGH / MAF translocations, provide useful prognostic information in PCM.
Because the malignant cells of plasma cell myeloma tend to grow poorly in culture, and some clinically-relevant abnormalities may be cryptic by metaphase cytogenetics, FISH analysis is generally preferred for cytogenetic evaluation of plasma cell myeloma.
Testing Recommendations for Plasma Cell Myeloma (PCM):
Chromosome Analysis: Bone Marrow
Flow Cytometric Immunophenotyping for Leukemia / Lymphoma
Fluorescence in situ hybridization (FISH) for:
• Plasma Cell Myeloma