Test Name
Fecal Occult Blood Test (IFOBT)
CPT Codes
82274
Methodology
Immunoassay (IA)
Turnaround Time
4 days
Specimen Requirements
Specimen Type:
Stool
Collection Container:
OC-Auto® FIT Personal Use Kit
Transport Temperature:
Ambient
Stability
Ambient:
15 days
Refrigerated:
30 days at 4°C
Frozen:
Unacceptable
Reference Range
Negative for hemoglobin at < 100 ng/ml
Additional Information
Background Information
In the United States, colorectal cancer is the third most common cancer diagnosed among men and women, and the second leading cause of death from cancer. Colorectal cancer can largely be prevented by the detection and removal of adenomatous polyps. Five-year survival is 90% if the disease is diagnosed while still localized, but only 68% for regional disease (a disease with lymph node involvement), and only 10% if distant metastases are present.1 In spite of this, a majority of U.S. adults are not receiving regular age- and risk-appropriate screening or have never been screened at all.2
There is a range of options for colorectal cancer screening that includes stool testing for the presence of occult blood or exfoliated DNA, or structural examinations that include flexible sigmoidoscopy, colonoscopy, double-contrast barium enema, and CR-colonography. Beginning in 1980, the American Cancer Society first issued formal guidelines for colorectal cancer screening in average-risk individuals and these have been periodically updated, along with additional guidelines for high-risk individuals.3 Other organizations, such as the American College of Radiology, U.S. Preventive Services Task Force, and the U.S. Multi-Society Task Force on Colorectal Cancer, have also issued recommendations. Collaborative efforts among these groups took place in 2008 to come to a consensus and provide joint guidelines and recommendations.1
Occult gastrointestinal bleeding refers to bleeding that is not apparent to the patient. It has traditionally been identified by tests that detect fecal blood, or, if bleeding is sufficient, as iron deficiency anemia. A variety of fecal occult-blood (FOB) tests have been designed primarily to screen for colon cancer, including both guaiac-based (gFOB) and immunochemical-based stool tests (iFOBT or FIT). The likelihood that FOB tests will detect gastrointestinal blood is affected by the type of test utilized, anatomical level of bleeding (upper GI vs. colonic), stool transit time, stool mixing, intra-luminal hemoglobin degradation, and features intrinsic to bleeding lesions (i.e. irregular bleeding).4
Clinical Indications
There are two major reasons to detect occult blood in the stool: as a screen for colorectal cancer or to detect upper or lower GI bleeding. In the outpatient settings, an immunochemical-based assay (iFOBT or FIT) is used to detect fecal occult blood for colorectal cancer screenings; the three-part guaiac-based fecal occult blood test will no longer be available for screening.
- The single guaiac card (SENSA) will continue to be used for the detection of bleeding (upper or lower GI bleeding).
- The iFOBT (FIT) cannot be used for detection of upper GI bleeding and should only be used as a colon cancer screen test.
- The HemaPrompt card (a guaiac-based POCT assay) was introduced in October 2009 for use as a point-of-care test for detection of upper and lower GI bleeding.
- It can be used in the Emergency Department and a few other clinical areas that have been granted POCT testing privileges.
If colorectal cancer screening is the intended use of the occult blood test, the iFOBT is the preferred method because it is the more-sensitive screen, and only a single sample collection is required.
One of the main reasons for the change to iFOBT for colorectal cancer screening is that the guaiac-based tests lack the sensitivity and specificity seen with the iFOBT assays. In an early study of iFOBT assays, specimens obtained from 107 colorectal cancer subjects showed that the iFOB test had a 97% sensitivity for detection of colorectal cancer, as compared to a very-sensitive guaiac-based test (Hemoccult Sensa) in which the sensitivity was 94%. The iFOBT also demonstrated greater sensitivity (76%) in detecting large adenomas as compared with guaiac-based tests, in which the sensitivity was 42%. The specificity of the iFOBT was 97.8%, as compared to 96.1% for the gFOB, when 1,355 screening tests were performed. The authors concluded that the iFOBT provided the best combination of specificity and sensitivity.5 In a more recent study of performance characteristics for detecting cancer, the sensitivity of the iFOBT test was 81.8% vs. 64.3% with gFOB test.
Specificity for iFOBT was 96.9% and 97.3%, respectively, for detecting cancer and adenomas versus 90% and 90.6% with gFOB. For the detection of large polyps, the sensitivity of the gFOB was actually higher than that with iFOBT in this study.6 In a recent study out of Seoul, Korea, a population of average-risk individuals (770 patients from four centers) undergoing colorectal cancer screening were assayed for occult blood comparing a gFOB to an iFOB. The iFOBT provided a higher sensitivity for detecting cancer and advanced colorectal neoplasia than the gFOB and had an acceptable specificity that could significantly reduce the need for colonoscopic evaluation of the screened population.7 An editorial in the same issue of the journal from Seoul suggested that the data supported an effort to increase the use of iFOBT assays in the U.S. and publishing of studies in average-risk individuals here as well.8
Secondly, various foods and exogenous substances can yield false-positive guaiac-based FOB test results. Vitamin C in excess of 250 mg/day from all sources (dietary and supplemental) can oxidize guaiac. False-positive guaiac-based test results can also occur with excess dietary red meat, such as beef, lamb, processed meat, liver, or plant peroxidases contained in raw fruits and vegetables, especially radishes, turnips, horseradish, cantaloupes, and other melons. Such foods should be avoided for 72 hours prior to testing. GI bleeding can be induced by alcohol, and also has well-known iatrogenic causes, such as steroids and NSAIDS.9
The iFOBT assays detect human globin, a protein that along with heme constitutes human hemoglobin. It is more specific for human blood as compared to the guaiac-based tests, and is not subject to the false-negative results seen in the guaiac-based tests in the presence of high dose vitamin C supplements. It is important to remember that the iFOBT assays are specific to bleeding in the lower GI tract.
Thirdly, because of the increased sensitivity of these assays, only one sample is usually required for screening, as compared to the three samples needed when guaiac-based tests are used. The ease of use of these screening assays should enhance patient compliance.
Interpretation
Positive:
Samples with a hemoglobin concentration >/=100 ng/mL
Negative:
Samples with a hemoglobin concentration <100 ng/mL
Because gastrointestinal lesions may bleed intermittently, and blood in feces is not distributed uniformly, a negative result may not assure the absence of a lesion.
Limitations
Patients with the following conditions should not be tested due to a potential for false positive results:
- Bleeding hemorrhoids
- Menstrual bleeding
- Constipation bleeding
- Urinary bleeding
Certain medications, such as aspirin and non-steroidal anti-inflammatory drugs, may cause gastrointestinal irritation and subsequent bleeding in some patients, which may cause false positive results.
Contamination of the sample with urine or toilet water also may cause erroneous results.
The OC-Sensor Diana iFOBT should not be used for testing urine, gastric or other body fluids.
Because iFOB (FIT) tests are dependent on the intact antigenic structure of heme molecules, its use is limited to screening for FOB that is not gastric or upper GI in origin.
Bulk stool samples should not be sent to the lab for occult blood testing, as hemoglobin present in stool begins to degrade within hours of passage.
Methodology
The OC-Sensor Diana iFOB test is an immunoassay-based test that uses rabbit polyclonal antibodies to detect hemoglobin in stool. The test is a turbidimetric latex agglutination test. Hemoglobin present in the patient sample will combine with latex-coated antibody to cause a change in absorbance. A light beam is passed through the reaction cells and measures changes in the intensity of light beam. Testing is performed on an automated analyzer and qualitative results are generated.
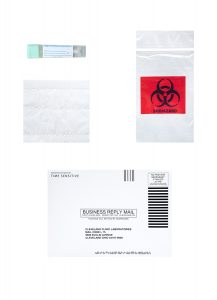
Patients should be provided with a collection kit, which is composed of a labeled collection vial, instructions on how to collect the stool sample and inoculate the vial, and an envelope into which the vial can mailed to the laboratories for testing.
Testing is performed on a daily basis, Monday through Friday
References
1. Levin B, Lieberman DA, McFarland B et al. Screening and Surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the U.S. Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Ca Cancer J Clin. 2008;58:130-60.
2. Smith RA, Cokkinides V, Eyre HJ. Cancer screening in the U.S., 2007: a review of current guidelines, practices, and prospects. CA Cancer J Clin. 2007;57:90-104.
3. Rex DK et al. American College of Gastroenterology Guidelines for Colorectal Cancer Screening 2008. The Am J Gastroenterol. 2009;104:739-50.
4. Rockey, DC. Occult gastrointestinal bleeding. N Engl J Med. 1999;341:38-46.
5. St. John DJ, Young GP, Alexeyeff MA et al. Evaluation of new occult blood tests for detection of colorectal neoplasia. Gastroenterology. 1993;104:1861-8.
6. Sakoda LC, Levin TR et al. Screening for colorectal neoplasms with new fecal occult blood tests: update on performance characteristics. J Natl Cancer Institute. 2007;99:1462-70.
7. Park D, Ryu S, Kim YH et al. Comparison of guaiac-based quantitative immunochemical fecal occult blood testing in a population at average risk undergoing colorectal cancer screening. Am J Gastroenterol. 2010;105:2017-25.
8. Allison JE. Editorial: FIT: a valuable but underutilized screening test for colorectal cancer – it’s time to change. Am J Gastroenterol. 2010;105:1026-8.
9. Bakerman, S. ABC’s of interpretive laboratory data. Fourth Edition. Interpretive Laboratory Data Inc. Scottsdale, AZ. 2002.