Special Communication
Send-out Test Discontinuation: Complement Factor B (C3PA)
Effective June 7, 2021
Test Discontinuation
Complement Factor B (C3PA)
At this time, there is no recommended replacement test.
At this time, there is no recommended replacement test.
Given coagulation testing’s critical role in many areas of medicine and surgery, Cleveland Clinic is implementing several supply conservation measures, including:

If a patient is not on anticoagulants or is not going to surgery:
Reconsider the need for routine coagulation testing or consider extending the interval between daily coagulation testing orders.
If a patient is undergoing treatment with direct oral anti-Xa anticoagulants, such as apixaban or rivaroxaban:
Consider not ordering PT and APTT (they are usually normal in these patients and not helpful in anticoagulant management).
Test Name
Order Code
# of 1.8 mL light blue tubes needed
# of 2.7 mL light blue tubes needed
# of 3.5 mL light blue tubes needed
Cleveland Clinic Laboratories will communicate further updates when available. Please continue to check our website or contact Client Services at 800.628.6816 for assistance.
Remove:
• (MUSBND) ACh Receptor (Muscle) Binding Ab
• (PARGAD) GAD65 Ab Assay
• (VGKC) Neuronal (V-G) K+ Channel Ab
• N-Type Calcium Channel Ab
• P/Q-Type Calcium Channel Ab
• Striational (Striated Muscle) Ab
• Reflex (MUSMOD) Muscle modulating antibody
• Reflex (CASRFX) CASPR2-IgG CBA
• Reflex (CRMPSX) CRMP-5-IgG
• Reflex (LG1RFX) LGI1-IgG CBA
• Reflex (PURK2X) Purkinje Cell Cytoplasmic Ab Type 2
Add to Panel:
• (CASRFX) CASPR2-IgG CBA
• (CRMPSX) CRMP-5-IgG
• (LG1RFX) LGI1-IgG CBA
• (PURK2X) Purkinje Cell Cytoplasmic Ab Type 2
Remove:
• (GANG3) AChR Ganglionic Neuronal Ab, S
• N-Type Calcium Channel Ab
• P/Q-Type Calcium Channel Ab
• Reflex (MUSMOD) Muscle modulating antibody
Remove:
• Striational (Striated Muscle) Ab
• N-Type Calcium Channel Ab
• Reflex (MUSMOD) Muscle modulating antibody
Add:
• Reflex (ACMFCS) AChR Modulating Flow Cytometry, S
Reason:
Discontinued by reference lab (Mayo Clinic Laboratories)
Alternative Test:
Myasthenia Gravis (MG)/Lambert-Eaton Syndrome (LES) Evaluation, Serum (MGLESE)
Reason:
Discontinued by reference lab (Mayo Clinic Laboratories)
Alternative Test:
Myasthenia Gravis Evaluation with Muscle-Specific Kinase (MuSK) Reflex, Serum (MYSGRV)
Beginning February 16 through May 16, 2021, specimens will be analyzed with both methods to establish a new baseline for individual patient results. Results from the previous method and reference intervals will be posted in a comment on the patient’s chart.
This change increases the detection of inhibin B in all clinically relevant cases and expands the testing range to improve sensitivity.
Additional details are available in the February 2021 Technical Update.

Female
1 day – 12 years:
1 – 182 pg/mL
13 – 41 years (regular cycle, follicular phase):
8 – 223 pg/mL
42 – 51 years (regular cycle, follicular phase):
1 – 107 pg/mL
51 – 76 years (postmenopausal):
1 – 11 pg/mL
Male
< 15 days:
68 – 373 pg/mL
15 days – 6 months:
42 – 516 pg/mL
7 months – 7 years:
24 – 300 pg/mL
8 – 30 years:
47 – 383 pg/mL
31 – 72 years:
10 – 357 pg/mL
ANSH ultrasensitive Inhibin B ELISA method
formerly Beckman Coulter Inhibin B Gen II ELISA method
Cleveland Clinic Laboratories is experiencing severe supply constraints for Stool Gastrointestinal Panel by PCR (STGIPR) testing. These shortages impact laboratories nationwide, resulting in the inability to identify a reference laboratory to forward this testing.

The tests listed below cover the range of pathogens detected in the Stool Gastrointestinal Panel by PCR (STGIPR) test. Depending on clinical circumstances and judgment, various combinations of these tests may serve as an appropriate substitution for STGIPR:
Test Code
Components
Performing Lab
STLPCR
Salmonella spp., Shigella spp., Campylobacter jejuni/coli, and Shiga-toxin (stx1 and stx2) genes
CCL
OVAPSC
Giardia lamblia and Cryptosporidium species
CCL
CRYSPO
Cryptosporidium, Cyclospora, and Cystoisospora sp.
CCL
OVAP
Cryptosporidium and Giardia
CCL
CDPCR
C. difficile toxin B gene
CCL
EROTA
Rotavirus antigen
CCL
VIBCUL
Vibrio
CCL
YERCUL
Yersinia
CCL
NORPCR
Norovirus 1 & 2
ARUP
SADNO
Adenovirus antigen
Focus
While supplies are constrained, culture and antigen testing will be used in place of PCR testing to interrogate specimens for the same pathogens as STLPCR: Campylobacter, Salmonella, Shigella, and Shiga toxin-producing E. coli (STEC/EHEC).
Cleveland Clinic Laboratories will temporarily cancel and credit any STLPCR test requests, then substitute clinically-equivalent culture and antigen testing.
The associated CPT codes for these substitutions are:
• 87449 (x 2)
• 87045






Specimen Type:
• Nasopharyngeal (NP) swab – preferred
• Nasal (anterior nares) swab
• Oropharyngeal (OP) swab
Specimen Type:
• Nasopharyngeal (NP) swab – preferred
• Nasal (anterior nares) swab
• Oropharyngeal (OP) swab
Specimen Type:
• Nasopharyngeal (NP) swab – preferred
• Nasal (anterior nares) swab
• Oropharyngeal (OP) swab
Specimen Type:
• Sputum
• Bronchoalveolar lavage (BAL)
*lower respiratory specimens only
Review our Coronavirus 2019 Testing Overview for additional details, including collection instructions, required patient demographics, and more.
If you are having difficulties obtaining appropriate COVID-19 specimen collection and transport supplies, please contact your CCL Account Manager.
Please contact Client Services at 800.628.6818.
Because of the severe shortage of urine tubes, providers should reserve urine testing for men with persistent urethritis. This practice aligns with guidance from the Centers for Disease Control and Prevention (CDC).

Ordering Options for Gonorrhea/Chlamydia Testing
Ordering Options for Trichomoniasis Testing
Although CCL cannot provide this item, Aptima tubes will continue to remain an acceptable specimen collection container for testing.
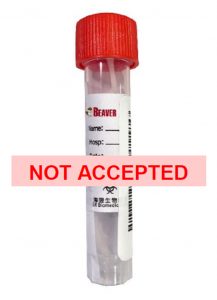
Because of the limited stability of unpreserved urine for gonorrhea, chlamydia, and trichomoniasis testing, Cleveland Clinic Laboratories is currently unable to accept urine in a sterile container (i.e., specimen cup) for UGCCT and TRVAMP orders.

Cleveland Clinic Laboratories will notify clients when Aptima urine tubes are back in stock and available to order. Conservative ordering practices may be necessary until supplies stabilize.
For help in prioritizing which patients to test for these pathogens, please refer to the recently-issued considerations from the CDC.